Description of INTEGRATE-Pain:
The National Institutes of Health (NIH) in the United States, including the NIH Pain Consortium and the NIH Helping to End Addiction Long-term Initiative (NIH HEAL Initiative), and the IMI-PainCare consortium of the Innovative Medicine Initiative (IMI), a public-private partnership for health between the European Union and European pharmaceutical companies, are dedicated to improving the understanding, management, and treatment of pain.
Both NIH and IMI-PainCare have common priorities in preclinical and clinical research, and collaboration between the two groups could help accelerate the discovery and development of new non-addictive treatments and improve the management of pain.
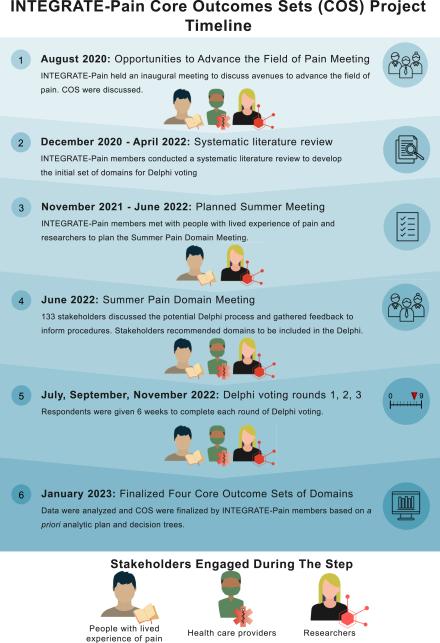
With the belief that collaboration can help lead to innovations in pain management, we established INTEGRATE-Pain, the “IMI-NIH Transatlantic Emphasis Group on Research And Translation-to-care Efforts for Pain.” In August 2020, the INTEGRATE-Pain Consortium held its inaugural meeting to discuss opportunities to advance the pain field and find areas of pain research that could benefit from cooperation. During the meeting, participants identified areas where collaboration could improve pain research and meaningfully impact the pain crisis throughout the world. These areas include standardized patient-reported outcomes (PROs), the use of biomarkers, and the standardization of reporting core outcome sets (COS), among others. Virtual workshops during the meeting highlighted the need for consensus between the U.S. and the EU on PROs to allow for the aggregation of data related to acute pain, chronic pain, the transition from acute to chronic pain, and episodic/breakthrough pain conditions.
The goals of the INTEGRATE-Pain Consortium are knowledge-sharing, harmonization of standards, combination of infrastructures, coordination of data collection to improve the statistical power of data interpretation in future meta-analyses, and joint dissemination. The Consortium has shared the results of published research within the U.S. and EU, discussed current projects and research ideas, and identified ways to advance the field of pain science. However, the Consortium does not discuss the creation or the development of future programs/funding announcements.
Of the opportunities and priorities that INTEGRATE-Pain has established in recent years, a recent area of focus is developing a consensus on a core set of patient-reported outcomes (PROs) for pain conditions (accounting for comorbidities). Both NIH staff and EU pain researchers were independently working on selecting and implementing common data elements (CDEs) for pain. As such, INTEGRATE-Pain performed a systematic literature review to identify pain-related COS throughout the world, and invited them to a virtual pain domain consensus meeting in June 2022 to discuss the need for overarching COS for the continuum of pain from acute to chronic pain. Over 150 people in pain research, practice, or experience living with pain participated in the virtual meeting, and participants voted in favor of creating four overarching COS for acute, acute to chronic, recurrent/episodic, and chronic pain. INTEGRATE-Pain therefore undertook a large international Delphi study from July 2022 to January 2023 to reach consensus on the most critical domains for each of the four aforementioned pain categories. The results of the study are available here.
INTEGRATE-Pain Delphi Process:
The image below* outlines the process of creating COS for pain, from the inception of the INTEGRATE-Pain consortium in 2020 to the finalization of the domains as a result of the international Delphi study.
This table* outlines the four different pain categories for which we created COS. The categories span the pain continuum, and the definitions were created in accordance with literature and agreed on by our advisory and steering committees and reviewed by meeting attendees.
|
Pain Category |
Definition |
Example Condition(s) |
|---|---|---|
|
Acute pain |
Pain experiences and conditions lasting for a relatively limited time, up to a few weeks, and generally remitting when the underlying pathology resolves; often occurs after trauma, surgical interventions, and some disease processes |
Acute post-operative pain, pain in labor, fracture, and ulcer |
|
Transition from acute to chronic pain |
Pain experiences and conditions lasting from a few weeks to three months |
Post-operative recovery |
|
Recurrent/episodic pain |
Pain experiences and conditions lasting for a relatively short time but recurring across an extended period |
Sickle cell-associated pain, migraine, polymyalgia rheumatica, and calcium phosphate deposition, dysmenorrhea |
|
Chronic pain |
Pain experiences and conditions lasting longer than three months |
Chronic low back pain, chronic postsurgical pain, chronic pelvic pain, and diabetic neuropathy |
The figure below* provides further details on the methods for achieving consensus on domains for the COS across the 3-round Delphi. The methodology for reaching consensus was informed by previous COS studies, guidelines from the COMET initiative, and advice from our advisory and steering committees. All decisions for eliminating and/or advancing domains were communicated to voters prior to each round of voting.
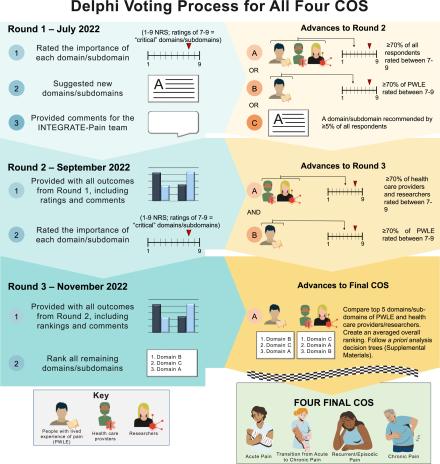
Summary of voting criteria for each round: During Delphi voting, we asked stakeholders to self-identify as either a person with lived experience (PWLE), or a researcher/clinician/other (R/C/O), and analyzed results based on the two stakeholder groups. During rounds 1 and 2, participants rated domains/subdomains on a Likert scale of 1-9, where 1-3 = not critical, 4-6 = important but not critical, and 7-9 = critical for inclusion into a COS. Domains/subdomains advanced to from round 1 to round 2 if >= 70 of all participants or >= 70% of PWLE rated them as critical (7-9). Voters also suggested domains, and were included in round 2 if >= 5% of the group recommended it. Domains/subdomains advanced from round 2 to 3 if >= 70% of PWLE and R/C/O both rated them as critical (7-9). For round 3, voters ranked their top 5 domains/subdomains of those that had advanced, and the research team created an average overall ranking score for each domain from the two groups of stakeholders to determine the top 5 domains for the final COS for each group.
Results of the INTEGRATE-Pain Delphi:
The international, online Delphi took place from July 2022 to January 2023. Over 450 individuals participated in the Delphi, with some individuals participating in more than one pain category. For a comprehensive explanation of the methods and results of the study, please refer to the published manuscript [pdf download link(pdf, 1321 KB)]: https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(23)00517-5/fulltext
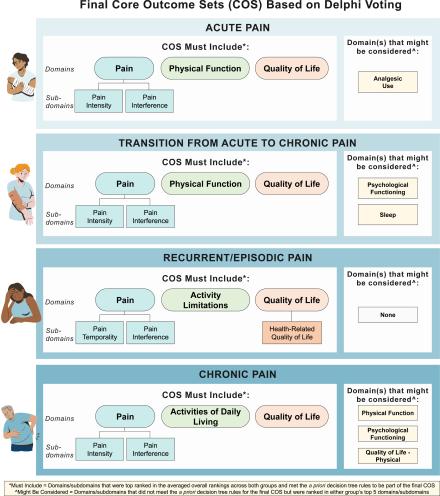
Below are the resulting core outcome sets (COS) of domains* for each of the four pain categories that span the pain continuum: acute, acute to chronic, recurrent/episodic, and chronic pain:
*Images and tables taken from: Bova G, Domenichiello A, Letzen JE, Rosenberger DC, Siddons A, Kaiser U, et al. Developing consensus on core outcome sets of domains for acute, the transition from acute to chronic, recurrent/episodic, and chronic pain: results of the INTEGRATE-pain Delphi process. eClinicalMedicine. 2023 Dec 1;66. DOI: https://doi.org/10.1016/j.eclinm.2023.102340
By sharing these results, we encourage all researchers studying pain or pain-related health conditions to consider measuring these domains, in addition to any condition-specific outcomes or measures that are relevant. Additionally, we hope that clinicians consider using these outcomes in their clinical practices while working with patients. If researchers and clinicians adopt these COS, the field of pain will likely benefit from greater comparability across studies and comparison of outcomes, thus increasing the likelihood of better treatments in the future.
INTEGRATE-Pain Delphi Stakeholders and Participants
The INTEGRATE-Pain steering committee would like to thank all individuals who participated in the Delphi by voting in any of the three rounds of surveys, with many individuals voting in multiple groups. This was a significant effort, and the input from stakeholders involved in this process was crucial to ensuring that the resulting core outcome sets reflected a wide range of perspectives from various disciplines, countries, and experiences living with pain.
Below are the names of individuals who were involved in the INTEGRATE-Pain project and/or participated in the online Delphi. The individuals listed below agreed to be acknowledged by name and provided written consent to have their name, degree, and affiliation listed below. Please note that the below list of individuals is not an exhaustive list of participants.
|
Name and Degree |
Affiliation |
|---|---|
|
Catherine Allaire, MDCM |
University of British-Columbia, Canada |
|
Adam Anicich, MBA |
NIH-DoD-VA Pain Management Collaboratory |
|
Ralf Baron, Prof. Dr. med. |
Division of Neurological Pain Research and Therapy, Department of Neurology, University Hospital of Schleswig-Holstein, Campus Kiel, Germany |
|
Marcus Bateman, BSc(Hons), MSc |
University Hospitals of Derby & Burton NHS Foundation Trust, UK |
|
Emine O. Bayman, PhD |
University of Iowa |
|
Joletta Belton, MSc |
n/a |
|
Bouche Bénédicte, MD |
n/a |
|
Dorthe B. Berthelsen, PT, MSc, PhD-student |
Section for Biostatistics and Evidence-Based Research, the Parker Institute, Bispebjerg and Frederiksberg Hospital, Copenhagen, Denmark AND Research Unit of Rheumatology, Department of Clinical Research, University of Southern Denmark, Odense University Hospital, Denmark AND Department of Rehabilitation, Municipality of Guldborgsund, Nykoebing F, Denmark |
| Judy Birch, B.ED | Pelvic Pain Support Network |
|
Peter Böhm |
n/a |
|
David Bornstein, MD |
GWU |
|
Jennifer Boyle |
n/a |
|
Krista Brecht, RN, BScN, MScN (A) |
McGill University Health Center |
|
Anne Burke, PhD |
Central Adelaide Local Health Network |
|
Deborah Bush MNZM, QSM, Dip Tchg |
n/a |
|
Willemina Campbell, BA, BEd, LLB |
UHN: Toronto Western Hospital, Patient Research Partner, Toronto, Canada |
|
Aidan G Cashin, PhD |
Centre for Pain IMPACT, Neuroscience Research Australia |
|
Giulia Emily Cetera, MD |
IRCCS Ca' Granda Ospedale Maggiore Policlinico, Milan |
|
Ben D. Chlapek, MS, MPA |
n/a |
|
Manon Choinière, PhD |
Université de Montréal |
|
Angie Clerc-Hawke, BMedSci |
Our Recovery Ltd |
|
Penney Cowan |
American Chronic Pain Association |
|
Mary Cowern, BSc (Hons) |
Patient Research Partner - UK |
|
Emma Cox, MSc |
Endometriosis UK |
|
Andrew J. Darzi, MD, MPH, PhD |
McMaster University - IMPACT (HEI) |
|
Annabel Dawson, MA, Ed |
PPI |
|
Guilherme AM de Barros |
n/a |
|
Susan Evans, MBBS, FRANZCOG, FFPMANZCA, PhD |
University of Adelaide |
|
Camile Farah, MDSc, FRACDS(OralMed), PhD |
Australian Centre for Oral Oncology Research & Education |
|
John T. Farrar, MD, PhD |
University of Pennsylvania |
|
Julie Fritz, PT, PhD |
University of Utah |
|
Niti Goel, MD |
Duke University SOM |
|
Katie M. Golden, Patient Advocate |
U.S. Pain Foundation |
|
Gunilla Göran |
ENFA Patient Representative |
|
Anders Gram-Hanssen, MD, PhD |
Copenhagen University Hospital |
|
Hanna Grol-Prokopczyk, PhD |
University at Buffalo, SUNY |
|
Dee Hartmann, PT, DPT |
Dee Hartmann Physical Therapy |
|
Charis Hill, BA |
n/a |
|
Alison Hoens, MSc, BScPT |
University of British Columbia |
|
Catherine Hofstetter |
OMERACT |
|
John Ingram, MD, PhD |
Cardiff University, Cardiff, UK |
|
Smriti Iyengar, PhD |
NINDS/NIH |
|
Anderson Peder Højer Karlsen |
Department of Anesthesia and Intensive Care Medicine, Bispebjerg and Frederiksberg Hospital, Copenhagen, Denmark |
|
Barbara Illowsky Karp, M.D. |
NINDS/NIH |
|
Francis Keefe, PhD |
Duke University |
|
Gary D. Klasser, DMD |
LSU School of Dentistry |
|
Magdalena Kocot-Kępska, MD, PhD, EDPM |
Medical College, Jagiellonian University, Krakow, Poland |
|
Albère Köke, Dr |
Maastricht University |
|
Erin E. Krebs, MD, MPH |
University of Minnesota, Minneapolis VA Health Care System |
|
Patrica M. Hubert, DNP |
ACPA |
|
Anaïs Lacasse, PhD |
University of Quebec in Abitibi-Témiscamingue (UQAT) |
|
Dale Langford, PhD |
n/a |
|
Eugenie Lee, BFA |
n/a |
|
Christine Lin, PhD |
The University of Sydney |
|
Chao Lu, DMD, BDS |
Tufts University, School of Dental Medicine, Craniofacial Pain Center |
|
Quana Madison, MA |
National Pain Advocacy Center |
|
Katie MacDonald |
n/a |
|
Nadia Malliou, MSc Cognitive Psychologist |
Pain Alliance Europe - PAE |
|
Paolo Martelletti, MD |
Unitelma Sapienza University of Rome |
|
Michelle Martin, Mpsych(Clin) |
n/a |
|
Stephanie Mathieson, PhD |
The University of Sydney |
|
Lara Maxwell PhD |
Faculty of Medicine, University of Ottawa, Canada |
|
Robert J. McCarthy, Pharm D |
Rush University |
|
Ewan McNicol, PharmD, MD |
Massachusetts College of Pharmacy and Health Sciences |
|
Amir Minerbi, MD, PhD |
Technion Israel Institute of Technology |
|
G. Lorimer Moseley, PhD |
Innovation, Implementation and Clinical Translation (IIMPACT) in Health, University of South Australia |
|
Cibele Nasri-Heir , DDS, MSD |
Rutgers School of Dental Medicine |
|
Lorna M. Neill, BSc (Hons Nat Phil) |
PMRGCAScotland |
|
Kate M. Nicholson, JD |
National Pain Advocacy Center |
|
Tom Norris, MPA |
American Chronic Pain Association |
|
Ajayi K. Oluwafemi, Mtech |
GSI, GAPPA, IASP |
|
Dorit Pud, Professor |
University of Haifa, Israel |
|
Caroline Pukall, PhD |
Queen's University |
|
Millie Quiñones-Dunlap, MLS |
US Pain Foundation |
|
Bethan Richards, FRACP, PhD |
Institute for Musculoskeletal Health, SLHD |
|
Julio Cesar Rosa-e-Silva, MD, PhD |
School of Medicine of Ribeirao Preto - University of Sao Paulo |
|
Manuel Roulaud, MSc |
PRISMATICS, CHU de POITIERS, 86000 Poitiers |
|
Anna Samson |
n/a |
|
Alison Sbrana |
n/a |
|
Grayson Schultz, MS |
n/a |
|
Saurab Sharma, PhD |
University of New South Wales |
|
Jaclyn Megan Sions, PT, DPT, PhD |
University of Delaware |
|
Kathleen Sluka, PT, PhD |
University of Iowa |
|
Konstanze E. Snyder |
n/a |
|
Nadia Soliman, PhD |
Imperial College London |
|
Cindy Steinberg, BA, BS |
Director of Policy & Advocacy, U.S. Pain Foundation |
|
Jennifer Stinson, RN-EC, PhD, CPNP, FAAN |
The Hospital for Sick Children |
|
Pamela Stratton, MD |
NINDS, NIH |
|
Pervez Sultan, MBChB, FRCA, MD (Res) |
Stanford University, Dept of Anesthesiology, Critical Care and Pain Medicine |
|
Bronnie Lennox Thompson, PhD |
University of Otago, Christchurch |
|
Patrick Tighe, MD, MS |
Executive Director, Quality & Patient Safety Initiative Association |
|
Rolf-Detlef Treede, Prof. Dr. Med. |
Heidelberg University, Germany |
|
Rachel Tremblay, MSc erg. |
Clinique d'adaptation à la douleur chronique du CIUSSS Centre-Sud-de-l'Île-de-Montréal |
|
Dennis C. Turk, PhD |
University of Washington |
|
Christin Veasley, B.S. |
Chronic Pain Research Alliance |
|
Katy Vincent, MRCOG, Dphil |
University of Oxford |
|
Kevin Vowles, PhD |
Queen's University, Belfast |
|
Johanna Vriezekolk, Dr. |
Sint Maartenskliniek, Nijmegen, The Netherlands |
|
Ursula Wesselmann, MD, PhD, DTM&H (Lond.) |
University of Alabama at Birmingham, Department of Anesthesiology and Perioperative Medicine, Division of Pain Medicine, Birmingham, AL, USA |
|
David A. Williams, PhD |
University of Michigan |
|
Anna Williams |
n/a |
|
Harriet Wittink, PhD |
HU University of Applied Sciences |
|
Sarah Woller, PhD |
NINDS/NIH |
|
Francesa Wuytack, PhD |
University of Angers, UMR 1085 |
|
Paul Yong, MD, PhD |
University of British Columbia |
|
Changhe Yu, PhD |
Dongzhimen hospital affiliated Beijing University of Chinese medicine |
|
Sigridur Zoëga |
Landspítali University Hospital; University of Iceland |
